If Your Fingers Abruptly Turn Pale, It Could Be a Sign of This Rare Condition
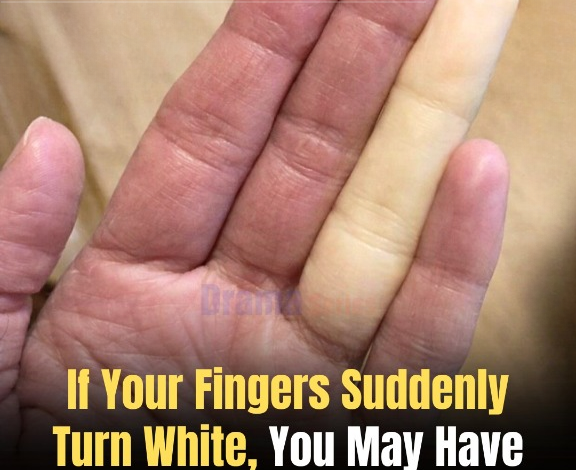
It can be a startling experience. One moment, your hands appear completely normal. The next, you notice one or more fingers turning an unusual color—chalky white, pale yellow, or even bluish-purple. At first, you might chalk it up to cold weather, especially during winter. But what if it keeps happening even when it’s not particularly cold? Or each time you hold an icy drink, or feel stressed?
In these situations, experts suggest that the cause might not be the temperature alone. You could be experiencing Raynaud’s disease, also known as Raynaud’s phenomenon.
What Is Raynaud’s Disease?
Raynaud’s disease affects blood circulation, most commonly in the fingers and toes. In some cases, it can also affect the ears, nose, lips, or even the nipples. During an episode—often called an “attack”—the small blood vessels in these areas suddenly narrow, a process called vasospasm, reducing blood flow.
When this happens, the skin can change color dramatically, typically following a pattern:
- White: Blood flow is restricted, causing the skin to lose its usual color.
- Blue: Reduced oxygen gives the skin a bluish tint.
- Red: As circulation returns, the skin flushes red, sometimes accompanied by tingling or throbbing.
Not everyone experiences all three stages, but even a single recurring color change can signal Raynaud’s.
Why Does It Happen?
The most common triggers are cold exposure and emotional stress. Even minor temperature changes can provoke an episode, such as:
- Holding a cold drink or can
- Reaching into the freezer
- Washing hands in cold water
- Walking from a warm indoor space into chilly air
Stress and anxiety can also trigger attacks, as tension can tighten blood vessels in a similar way to cold exposure. While the exact cause isn’t fully understood, researchers believe Raynaud’s involves an overreaction of the nervous system that regulates blood vessel constriction.
Primary vs. Secondary Raynaud’s
Raynaud’s is usually categorized into two types:
- Primary Raynaud’s (Raynaud’s disease): The more common, generally mild form, occurring on its own without an associated medical condition. Symptoms often begin in teens or early adulthood. While uncomfortable, primary Raynaud’s rarely causes lasting damage.
- Secondary Raynaud’s (Raynaud’s phenomenon): Linked to underlying conditions, often affecting connective tissue or blood vessels. This type tends to be more severe and may lead to complications, so doctors typically recommend further testing.
What Does It Feel Like?
Along with color changes, Raynaud’s episodes can produce:
- Cold fingers or toes
- Numbness or tingling
- A “pins and needles” sensation as blood returns
- Mild to moderate pain in some cases
For many, the most unsettling aspect is not the discomfort, but the sudden, dramatic appearance of their hands or feet.
Is Raynaud’s Dangerous?
For most with primary Raynaud’s, it is more of an inconvenience than a serious health risk. Episodes are temporary, and normal color and sensation usually return once the trigger is removed.
However, frequent or severe attacks—especially those causing pain, sores, or slow-healing wounds—should not be ignored. Prolonged loss of blood flow can, in rare cases, damage tissue. This is more likely with secondary Raynaud’s, making medical evaluation important if symptoms worsen or become intense.
How Is It Diagnosed?
There is no single test for Raynaud’s. Diagnosis usually relies on:
- A detailed account of symptoms
- Timing and frequency of episodes
- Identifying triggers
- Physical examination
If secondary Raynaud’s is suspected, additional tests may be ordered to identify underlying conditions. The aim is to understand not just what is happening, but why.
Managing Raynaud’s in Daily Life
While there is no cure, many manage symptoms successfully through consistent lifestyle adjustments:
- Keeping warm: Gloves, warm socks, and layered clothing help.
- Avoiding sudden temperature changes: Gradual warming or cooling prevents attacks.
- Managing stress: Relaxation techniques, deep breathing, and mindfulness can reduce stress-related episodes.
- Protecting hands: Using insulated cups for cold drinks or gloves when handling cold items can help.
In more severe cases, doctors may prescribe medications to relax blood vessels and improve circulation.
When to See a Doctor
Medical advice is recommended if:
- Color changes are frequent or severe
- Only one hand or finger is consistently affected
- Pain, sores, or skin breakdown occur
- Symptoms appear later in life or worsen suddenly
These signs may indicate secondary Raynaud’s or another circulation problem requiring attention.
The Bottom Line
Seeing your fingers turn white or blue can be alarming, especially when it happens without warning. While cold often triggers the episodes, repeated occurrences—particularly in response to minor temperature changes or stress—may indicate Raynaud’s disease.
The good news is that, for most people, Raynaud’s is manageable. With awareness, practical lifestyle adjustments, and medical guidance when necessary, most can continue living full, active lives without letting color changes control their day.